Anatomy and Symptoms
Back Pain and Sciatica
 Back pain is so common it is not so much a disease as a condition of life. The evidence of the elderly is that virtually all of us will suffer from it at some point. It is usually a passing phase and although it may bother you for a decade or more, if you are a young sufferer you should not presume that you will be in terrible and increasing trouble as your years role on. Rather than progress, it may instead resolve or plateau at an acceptable level.
Back pain is so common it is not so much a disease as a condition of life. The evidence of the elderly is that virtually all of us will suffer from it at some point. It is usually a passing phase and although it may bother you for a decade or more, if you are a young sufferer you should not presume that you will be in terrible and increasing trouble as your years role on. Rather than progress, it may instead resolve or plateau at an acceptable level.
For those of you who have developed a significant problem, you are at least not alone. In the UK each year, 2 million people attend their general practitioner with spinal problems, over 300,000 are referred for specialist care, over 60,000 are admitted to hospital and more than 30,000 people undergo surgery with many more having spinal injections (visit The Spine Surgery London website for more information about spinal injections). It is the single commonest cause of lost working days. The direct and indirect costs run into billions of pounds.
The causes of chronic back pain are many though by far the commonest is “degenerative disease” (visit The Spine Surgery London website for more information about degenerative disease). This degeneration is the normal process of wear and tear that occurs with life. It affects the discs, bones, joints and ligaments of the spine. If it arose anywhere else in the body it would be called arthritis though medics tend to call it “spondylosis” so as to create an air of mystique amongst the patients and to leave their students in a state of awe. There is more to it than just “wear and tear” for whilst it is more common amongst those who do heavy manual work or play heavy spinal sports such as rugby, there are many sedentary sufferers. There are familial patterns of inheritance, the random genetic lottery of our make-up and specific injuries adding to the mix as well as yet unidentified biological processes.
This degenerative process arises earlier in the spine than in any other joint of the body, frequently being seen on MRI scans in the late teens. This is not surprising when one considers the complexity of the spine, its mobility and the amount of weight that the lower segments take.
The spine consists of 24 bones, 23 discs, 46 major (facet) joints, in addition to 55 other smaller joints. The discs are merely modified joints and each joint consists of capsules, linings and cartilage (visit The Spine Surgery London website for more information about the spine).
The two main joints at each level are the facet joints. These are a pair of joints, just behind the spinal canal, one on either side. The surface of each joint is about the size of an adult little finger nail in area. The joints are supported by ligaments attached to the bones on either side of the joints. The main strength of the spine comes from its muscles which are in two groups; those which directly surround it like the erector spinae (lamb chop / T bone) or psoas (fillet steak) and those that work on the spine from afar such as the abdominal and pelvic floor muscles. This latter group are often called the core muscles.

The Basic Anatomy
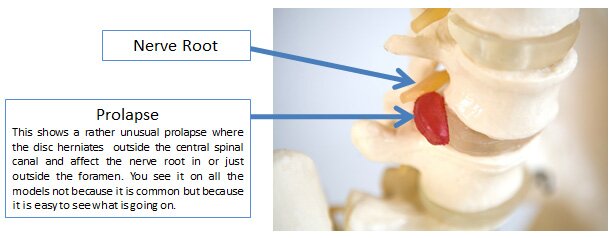
You can see from above that the bones of the spine are called vertebrae. There are five lumbar bones stacked on top of the sacrum and numbered L1 to L5 from the top down. The sacrum is a fused mass of vertebrae which coalesce as we develop in the womb. The top part of the sacrum is called S1 but this is fused/joined to S2 and S2 to S3 and so on. The iliac wing of the pelvic bone attaches to the spine at the sacroiliac joint on either side. Between each vertebrae is a disc. You can see the numbering of the discs relates to the vertebrae they lie between. So too does the numbering of the nerve root foramen. However, the nerve roots have their own numbers. Confusingly, these are the same as the bones – again L1 to L5. Look at the figure and see if you can follow the next sentence – if you get it you can be a doctor. Commonly a prolapsed disc will catch the nerve root which exits at the foramen below, i.e., an L4/5 prolapsed disc will compress the L5 nerve root which exits the central spinal canal below at the L5/S1 foramen. This nerve goes down the leg to the big toe which it supplies with power and sensation. So, the patient gets pain in the back from the disc and pain in the leg radiating to the toe from the from the nerve pressure. If it is bad, they will get numbness of the big toe and an inability to cock the big toe up – and if you get that you can be a spine surgeon!
The degeneration of the spine seen on MRI scans principally affects the discs and joints and for nearly all sufferers predates the onset of symptoms.
Terminology

There are some terms that are worth learning. “Degenerative spinal disease” is an umbrella term to refer to all the processes we are discussing here. As good as any catch all phrase, it correctly gives the impression that the process is inevitable and is related to age. Indeed, this is why we all get shorter, stooped and stiff as time goes by.
The incorrect impressions this phrase gives are as follows.
It is not confined to the elderly. If you study people in their late teens and people in their early 20’s you will see signs of it on their MRI scans. It does get more common as we get older – 50 year olds have more than 30 year olds on average – but there is a huge variation. Just as some men start balding before they turn 20 and others have full heads of hair until 70, there is a trend but only one with wide variations.
In addition, whilst it may begin earlier than degeneration or arthritis in the hips and knees, it is not as relentless in its progression. Degenerative problems may plateau or improve in the spine whereas in other joints the tendency is to deteriorate progressively until the joint is replaced. In the spine, a disc may wear out until it is so thin and stiff that it stops moving and then the pain goes away. “I had terrible trouble when I was in my fifties but now it is better”.
The degenerative process affects all different elements of the spine; the discs, the facet joints as well as the ligaments and muscles.
The facet joints tend to swell. The discs lose water and hence height, become weak and the disc capsule may rupture allowing the central pulp to herniate or prolapse through and then perhaps press on the nerve roots. Bony growths, called osteophytes, may grow off the discs and joints to the point that they too compress the nerve roots. Often sciatica (visit The Spine Surgery London website for more information about sciatica) derives from both a prolapse and an osteophyte narrowing occurring at the same level. As the ligaments degenerate they get thicker and add to these problems. The muscles get thinner and weaker with time and able to offer less protection to a by now vulnerable spine.
“Wear and tear” is another phrase used to mean the same thing as degenerative disease. This belies the fact that some of us get it earlier than others and whilst it is commoner in manual labourers and sports people, it is still common in office workers and the sedate.
Don’t be confused:
- A “slipped disc” is the same as a prolapsed, herniated or ruptured disc.
- Wear and tear is the same as degenerative and both are the same as “arthritis”
- “Spondylosis” is the medical word for arthritis when it affects the spine.
Back Pain

Back pain arises when inflammation occurs in these worn joints and discs. You cannot see the inflammation on the scan. You can see a similar process when you sprain your ankle. The initial injury hurts but the real pain and swelling develops over the following hours and days. The ankle becomes red, hot and angry. Similarly, in the spine an injury to any of the joints or discs may be minor – “I felt a tweak in my back” - but then slowly inflammation develops in the tissue which “tweaked” and pain builds. The provoking event may be trivial – “I reached over to grab an envelope of the back seat and felt a tweak, I had a back ache that night but woke up in agony”
Thus, back pain may be thought of as inflammation arising on a long-term background of wear and tear in the joints and discs of the spine (arthritis or aging).
Two common patterns arise:
In the first, the process is chronic and ongoing and symptoms are relatively constant and persistent – “continuous low back pain/ache” (CLBP). The pain is generally provoked after exercise, made worse by prolonged sitting or driving and is often worse in the morning especially after a heavy day. It gets worse as the working week goes on.
In the second, the episodes of inflammation wax and wane, often with dramatic onset in a pattern sometimes called “acute relapsing low back pain” (ARLBP). A trivial normal action, often as benign as bending over to pick up the soap or tie a shoe lace, triggers a tweak which develops over the following hours into incapacitating back pain. Some may even an instantaneous agony that leaves them crawling for the bed. The attacks may last a few days or a few weeks and will often begin with episodes occurring once every few years. Patients describe an absolutely normal pain free life being intermittently placed on hold.
As time passes, they may fail to fully resolve so there is an element of continuous low back pain and the frequency escalate into episodes every few months. Some get into a severe episode which will not settle.

Sciatica
Sciatica or leg pain emerges when the nerves servicing the legs, which pass through the spine, are compressed by the swollen joints or bulging (slipped/herniated/prolapsed) discs or irritated by inflammation in theses joints and discs.
Sciatica is therefore called a “referred pain” and arises because the pressure excites the nerve and the brain thinks anything that comes from that nerve comes from the leg.
There is another type of referred pain that comes from our internal organs not being localised well. Hence, we feel heart pain in our left arm. This is not because the heart presses on a nerve going to the arm but as a result of the brain incorrectly localising the heart in the arm.
Both types of referred pain occur in the spine as disc, facet joint or bone pain may be poorly localised to the groin, the buttocks and hips. Likewise, if you press on a nerve in the spine it does not always go all the way down the leg to the calf or foot. Any pain felt centrally in the back is due to the discs, bones or joints of the spine hurting themselves.

Any pain felt below the knee comes from the nerves being pressed on. A common pattern is to have pain in the back from a prolapsed disc and pain in the calf from the pressure the prolapse places on the nerve root. Pain felt to one side of the spine, in the buttock or down the leg to above the thigh is in “everyman’s land” and may reflect poor localisation or limited referral.

Why separate back pain and leg pain?
It is because the treatment is as different as the origin of these two pains. We need to understand where each element of your problem comes from.

It is the job of your doctor/us and is done by analysing your symptoms, their history, the examination findings and the tests- scans etc. It is only then that the treatment of the identified underlying problems can begin.
 |
An MRI scan showing an L4/L5 prolapsed intervertebral disc. The fact that the disc ruptured will cause acute low back pain. This gets worse as the inflammation builds. The bulging of the disc then squashes the nerve root and the inflammation in the disc irritates the nerve root. The leg pain, or sciatica, is due to the pressure from the prolapse and the inflammation it causes. It is rather like it is being pressed on by an iron which is turned on – “ouch, that hurts”
|
In broad terms, nerve root pressure, (i.e., leg pain), is best treated with rest and passive gentle treatments whereas back pain is best treated with active exercise bases treatments.
With this understanding of the mechanisms of the back pain and sciatica, a programme of conservative therapy can be addressed.